A Dermatologist’s Guide to Impetigo—From Experience
Video Transcript:
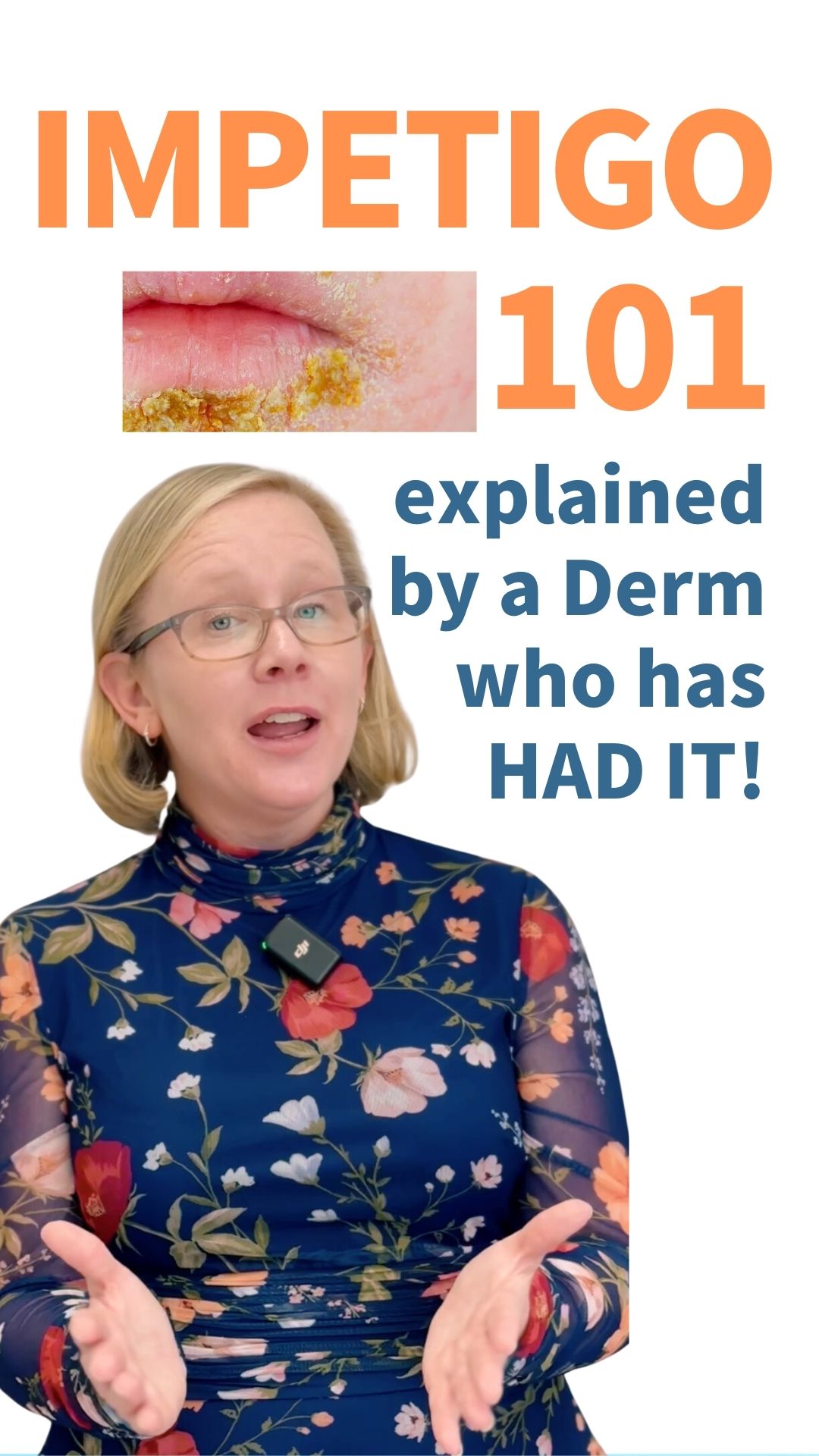
Impetigo is one of the reasons I went into dermatology. I got impetigo when I was in college. I was a college freshman, and I started developing this rash on my face shortly before Thanksgiving break. I was freaking out about it and had my parents schedule an appointment for the Friday after Thanksgiving so I could get it looked at.
I flew home Wednesday night, the night before Thanksgiving, and I had makeup on, so nobody really noticed anything. I went right to bed. Thursday morning, I woke up to have breakfast with the family that loves me, and they said, “What on earth is going on with your face?” It was not pretty. It was not pretty.
Fortunately, dermatology to the rescue! I saw my dermatologist on Friday. She took one look at me and said, “Oh gosh, this is impetigo, but we can manage it.” She got me started on an oral antibiotic, a topical antibiotic, and some vinegar soaks. I was better by the time I went back to college on Monday.
Treatment for impetigo is very effective and works rapidly when you’re on the appropriate treatment. Impetigo is a superficial skin infection caused by either staph or strep bacteria. Staph is the most common, and strep is the second most common. These bacteria are all around us—they live among us. It just takes one little break in your skin and being in the wrong place at the wrong time for that bacteria to set up shop and fester. Then, it spreads from spot to spot on a person once they have it.
It’s easy to diagnose. We can typically diagnose it visually, but if needed, we can do a swab culture to confirm the bacteria responsible. I typically like to do a swab culture because I want to know which bacteria it is and ensure it’s not resistant to any antibiotics I might want to use. While the culture is processing, we can start treatment to get people looking and feeling better very quickly.
A relatively common oral antibiotic we use is called cephalexin. It treats both staph and strep, making it a good choice. We typically also prescribe a topical antibiotic, mupirocin, to use two or three times a day. Back when I had impetigo, my dermatologist had me do vinegar soaks, which I found extraordinarily effective. I usually recommend them to my patients as well.
Here’s how to do vinegar soaks:
- Mix 1 part vinegar with 4 parts water in a bowl.
- Dampen a paper towel in the solution and drape it over the affected area.
- Let it sit for 10 to 15 minutes.
- Remove the towel, pat the area dry, and apply the topical antibiotic.
I really felt like it helped me get better faster because it removed the crust and helped the topical antibiotic penetrate better. So, I encourage vinegar soaks for my patients with impetigo, as long as they’re willing to put in the time.
Impetigo is interesting because it’s a very impressive rash, but often, there are little to no symptoms associated with it. You look at it, and it seems like it should hurt, but typically it doesn’t. When I had impetigo, maybe there was a slight tingle at times, but it was really the appearance that bothered me more than any symptoms.
Impetigo and the cold sore virus can look very similar. In fact, they can appear almost identical. In situations where I’m not sure, I perform a swab culture for both. You can swab for the bacteria that causes impetigo and the virus that causes cold sores. While waiting for the results, I start treatment for both conditions. That way, my patient gets better in the meantime, and the culture results later confirm the exact cause.
Impetigo is most common in younger patient populations—kids and teenagers are the classic demographic. I was a little older than usual when I had it, being in college, but I think I was meant to be a dermatologist. My experience with impetigo inspired me to pursue dermatology because I saw how quickly my own dermatologist was able to help me with what felt like a mortifying facial rash. I thought, “Wow, this dermatology stuff is awesome. This is something I want to do.”
Untreated, impetigo spreads rapidly. You can see it happen in real time. Over the course of a day or two, new spots appear. It can be psychologically devastating for patients or parents of kids with impetigo because every time you look, there’s a new spot. It evolves right before your eyes.
Impetigo should always be treated by a medical professional. It’s very uncommon for it to resolve on its own or with home remedies alone. I’m a big fan of vinegar soaks for treating impetigo, but only in combination with proper medications like oral and topical antibiotics. The soaks are a helpful addition but not enough by themselves.
Recurrent impetigo is not common, but if I meet a patient with a history of recurrent episodes, I start to wonder if it was actually cold sores. Cold sores commonly recur, so I might ask them to call me when they have a new spot so I can swab and confirm.
As someone who had impetigo in college, I went through a paranoid phase, constantly fearing it would return. I worried about it for three or four years, but recurrence is actually rare. One reassuring aspect is that impetigo usually doesn’t scar. Even though it looks severe, the infection occurs so superficially in the skin that it doesn’t reach the deeper layers that cause scarring.
The good news is that impetigo is treatable, resolves quickly with the right care, and rarely leaves a lasting mark.